With America facing the greatest income gap since the Great Depression, the largely unpublicized link between financial inequality and drug addiction suggests big trouble ahead.
For decades now, we’ve branded addiction “an equal opportunity disease.” And judging from the largely white, middle-class people who populate most AA meetings and rehabs, it is. 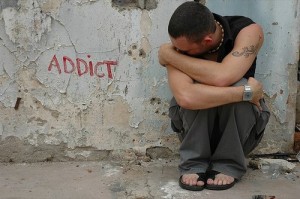
But while no sector of society is immune from substance abuse, addiction does discriminate. Examples abound: “drug problems” among college grads is nearly a third lower than those for high school dropouts, according to the National Household Survey on Drug Abuse and Health. Unemployed people are twice as likely to be addicts as people with jobs. With America facing the greatest income gap since the Great Depression, the largely unpublicized link between financial inequality and drug addiction suggests big trouble ahead.
Of course, the causal connection between poverty and substance use runs both ways. People who are suffering from alcohol or drug problems are obviously more likely to drop out of school or lose their jobs, while those who don’t have the education and skills to find a job in this fast-changing, increasingly high-tech economy not only increase face increased odds of addiction but also dramatically lower odds of recovery.
Stigma keeps addiction low on the list of “causes”; if, for purposes of raising funds and sympathy, the public face of recovery looks most like the people who have the resources to donate—with a celebrity or two thrown in—what’s the beef?
For example, Americans earning less than $20,000 a year are half as likely to successfully quit smoking—and nearly one third less likely to end a cocaine addiction—than those making $70,000 a year or more.
The recovery community has typically shied away from acknowledging these inconvenient truths. For one thing, addiction is so painful and destructive—and sobriety so difficult and one-day-at-a-time—that distinctions based on class or race can seem churlish. For another, stigma keeps addiction low on the list of “causes”; if, for purposes of raising funds and sympathy, the public face of recovery looks most like the people who have the resources to donate—with a celebrity or two thrown in—what’s the beef? Still, among ourselves, we need to admit the truth: addiction is disproportionately concentrated among the poor, and, consequently, among blacks and Hispanics.
Social problems plaguing the poor are largely ignored as intractable, a given of the invisible “underclass.” But as more and more Americans in the middle class become poorer, if not impoverished, by our ongoing economic crises—the implosion of the financial industry (goodbye IRAs and retirement funds), the raft of foreclosures and 10% unemployment (farewell to the bedrock American belief in a house and a job)—denying the link between income and addiction keeps us from finding workable solutions for the explosion in addictive behavior all around us. The most potent anti-craving medications in the world won’t prevent relapse among people who lack skills, job opportunities and hope.
It’s important to emphasize that drawing attention to the increased vulnerability to addiction that poverty poses is in no way meant to pit addict against addict or to sew discord. There are all too many middle-class and rich people in this country battling various addictions. But if we continue to ignore the special role that the lack of education and employment play in fermenting the growing drug problem, we are likely to leave them out of the solution when it comes to crafting treatment and prevention.
Instead, we need to address the specific social and economic problems that have made the US one of the most drugged-out countries in the world. The magic-wand policy answer would be, of course, to cut economic inequality. Almost without exception, nations, and even US states, where the concentration of wealth is greatest have not only more addictions but also more obesity, heart disease, stroke, mental illness and other major health problems than those with less inequality. The greater the inequality, the higher the murder rate, too.
These differences relate not to overall amount of wealth in industrialized countries but to how the money is distributed among the population. So why does inequality per se have such a profound impact on health, including addiction?
Like other primates, humans are hierarchical creatures: there are alphas and betas and so on down the line for both males and females. However, humans also have an innate desire for fairness. The reason children are so quick to say, “That’s not fair,” when their siblings get what seems to be a bigger piece of cake is not because parents teach them to measure their portions but because our brains predispose us to prefer at least some degree of equality—or at the very least rational explanation of unfair distributions.
Numerous studies demonstrate this preference. A major study conducted by the noted Duke University economist and author Dan Ariely found that Americans would favor a system of wealth distribution closer to the one found in Sweden (one of the world’s most egalitarian countries) than the current status quo in the United States. The 5,522 participants surveyed tended to believe that our existing wealth distribution was much closer to equitable than it is—before the crash made us much more aware of the reality.
Study after study has also found that people will pay to punish others who treat them unfairly, even when it isn’t in their own economic interest to do so. While people obviously often selfishly seek their own individual advantages, the idea that we prefer a Darwinian “dog eat dog” world over one in which people have a fair chance at winning through hard work is simply not supported by the data. We’re hierarchical, but we also crave justice. 
This is probably related to the fact that we evolved in tight-knit, highly egalitarian groups in which selfishness was highly discouraged because survival required cooperation. Whatever the case, even in the most egalitarian societies, there is a survival difference between those on top and those on the bottom. But that difference is greatly magnified when economic inequality is high. A stress abuse of mortality among all human beings is stress, which is the primary factor in a long list of fatal illnesses. By and large, wealthier people are more equipped to insulate themselves from the stressors of daily life. But people in poverty suffer through a much the greater degree of uncertainty and insecurity, both of which exacerbate chronic stress. Even at the top of the financial pyramid, however, competition, responsibility, and fear of failure take a constant toll.
Meanwhile, chronically elevated stress hormone levels increase the risk of virtually every illness you can name: not just addictions, obesity, diabetes and cardiovascular disease, but also infectious diseases, infant mortality and most cancers.
In one famous study of British civil servants, people on the bottom rung of the hierarchy suffered mortality rates three times higher than those on the top at every age—and the difference was graded sequentially from top to bottom. Only about one third of the difference in death rates was accounted for by factors like smoking and obesity—the rest was caused by the stress itself, not self-medication to try to cope with it.
Keep in mind that those on the bottom weren’t unemployed or even poor: they were working class, and because Britain has a national health care system, their worse health was not due to lack of access to medical services. Further, the US is even more unequal than the UK: in America, the ratio of CEO to worker pay is now 185 to one; in Great Britain, that figure is 28 to one (and they’re considered one of the most inequitable countries in Western Europe).
Although direct comparisons between countries on rates of drug problems are hard to make, one 2003 study contrasted rates of active drug dependence (the DSM diagnostic term for “addiction”) among Americans to that of Brits. It found a drug dependence rate of 1.5% in the U.S. and 0.5% in the UK: three times lower.
America, as many of us may remember, used to be far less unequal: in the postwar years from 1948 to 1985, on average, annual American income grew by $21,162. Some 60% of that growth went to the bottom 90% of earners. In contrast, between 1986 and 2008, average yearly take-home grew by a mere $6,894—and 100% went to the top 10%. In fact, on average, the income for 90% of Americans declined.
If we want to fight addiction, these numbers and trends are unsustainable. Reducing inequality isn’t just a boon to the middle class and poor—it could help every level of society by raising educational achievement, cutting health costs, crime, criminal justice expenditures and stress.
Obviously, this would require more taxes on the wealthy and on corporations and greater spending on schools, particularly early childhood care. It would require a commitment to genuine equality of opportunity—not of outcome, but of real options.
Alternatively, we can continue to self-medicate with food, cigarettes, alcohol, heroin, coke, meth, oxy, sex, the Internet—the list of consumer goods employed in a failing attempt to alleviate stress without getting to its root causes keeps growing—and go on fighting an endless, equally failing, war on drugs—and on ourselves.
 sending...
sending...

[...] is also known to discriminate, with unemployed people being twice as likely to develop [...]